File a Claim
Billing & Claims
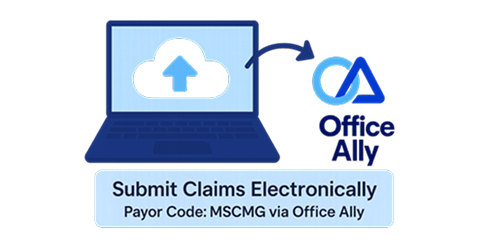
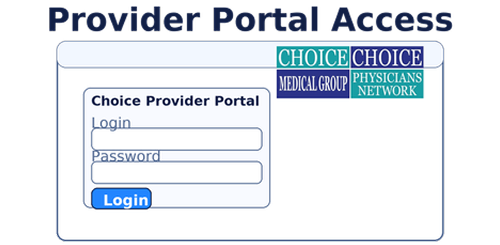
Claims administration including intake, status checks, denials, remittance/EOBs, and reconsiderations or appeals is handled by Choice Physicians Network and MHM Health, our Management Services Organization, through the EZ-NET portal.
Payments come from MD Senior Care Medical Group, the IPA. Funds are released after claims are approved by the MSO according to our delegation. Therefore, please work with Choice/MHM Health for all claim submissions, status inquiries, remittance copies, denials, and appeals.
Note: MD Senior Care Medical Group handles contracting matters or clinical issues that are not related to claims processing.


%201.png)